Silicone Dilators for Pelvic Health: A Complete Guide
Pelvic health is a cornerstone of overall well-being, yet it remains shrouded in stigma and neglect. For millions worldwide, pelvic floor disorders—such as chronic pain, muscle dysfunction, and post-surgical complications—significantly impair daily life. As an industry expert with over 18 years+ in medical silicone devices manufacturing, JESilicone has seen silicone dilators emerge as a game-changer in this field. These devices, crafted from medical-grade silicone, offer a gentle, non-invasive approach to restoring pelvic function. Unlike traditional methods that may rely on medication or invasive procedures, silicone dilators empower individuals to take an active role in their recovery.
This guide delves into the science, applications, and best practices surrounding silicone dilators. By blending clinical evidence with practical insights, we aim to demystify these tools and highlight their role in promoting pelvic wellness. Whether you are a patient seeking relief or a clinician enhancing your toolkit, this article will serve as a comprehensive resource. The journey to pelvic health often begins with education, and understanding silicone dilators is a pivotal step toward empowerment and healing.
Table of Contents:
Understanding Pelvic Health: Why It Matters
What Are Silicone Dilators? A Detailed Overview
Benefits of Silicone Dilators for Pelvic Health
Conditions Treated with Silicone Dilators
How to Choose the Right Silicone Dilator
Step-by-Step Guide to Using Silicone Dilators Safely
Integrating Silicone Dilators into Pelvic Floor Therapy
Common Myths and Misconceptions About Dilators
Expert Tips for Maximizing Results
Frequently Asked Questions (FAQs)
Conclusion: Empowering Your Pelvic Health Journey
Understanding Pelvic Health
Pelvic health refers to the optimal functioning of the pelvic region, encompassing muscles, nerves, and organs like the bladder, uterus, prostate, and rectum. The pelvic floor muscles, a network of tissues stretching from the pubic bone to the tailbone, act as a supportive sling. They play crucial roles in urination, defecation, sexual activity, and stability.
When compromised, pelvic floor dysfunction can manifest as urinary incontinence, pelvic organ prolapse, chronic pain, or sexual disorders. Factors such as childbirth, aging, surgery, obesity, and sedentary lifestyles contribute to these issues. For instance, childbirth can stretch or tear pelvic muscles, while prostate surgery may weaken urinary control. The psychological impact is profound, with many individuals experiencing anxiety, depression, or social isolation.
According to the National Institutes of Health, nearly 25% of women and 10% of men suffer from pelvic floor disorders, yet underreporting persists due to embarrassment. Proactive management is essential—through exercises like Kegels, dietary adjustments, and tools like silicone dilators. By prioritizing pelvic health, we not only alleviate symptoms but also enhance quality of life. This section underscores the importance of awareness, early intervention, and holistic care, setting the stage for why silicone dilators are a valuable adjunct in treatment.
What Are Silicone Dilators?
Silicone dilators are cylindrical medical devices designed to gently stretch and desensitize pelvic tissues. Made from 100% medical-grade silicone, they are soft, flexible, and hypoallergenic, making them ideal for sensitive areas like the vagina or anus. Historically, dilators were crafted from rigid materials like plastic or metal, but silicone innovations have revolutionized their comfort and safety.
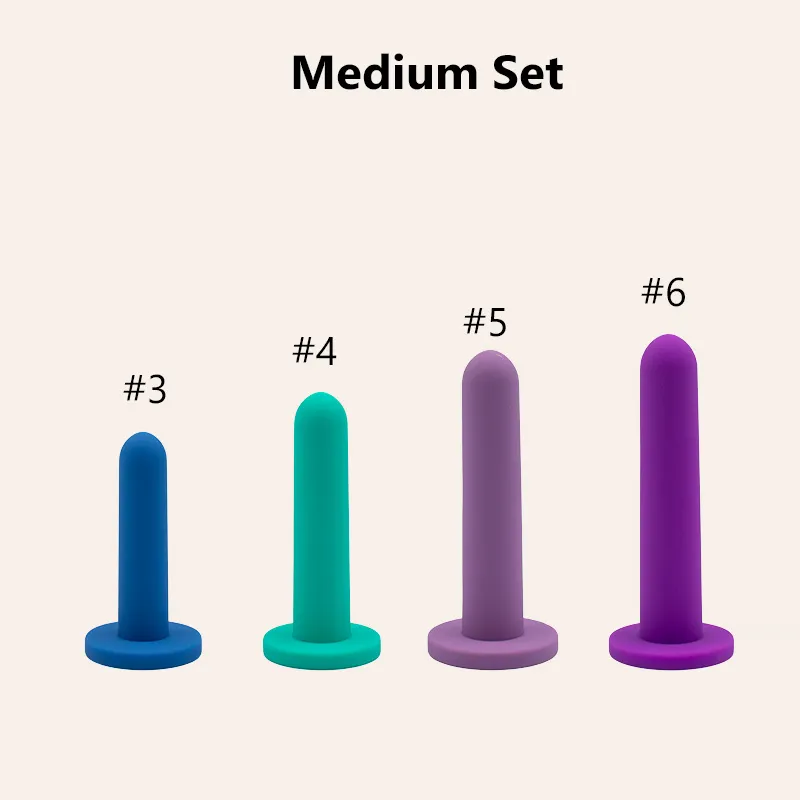
These dilators typically come in sets with increasing diameters—from as small as 0.3 inches for beginners to over 1.5 inches for advanced users. Their primary mechanism involves gradual progression: by inserting larger sizes over time, users can reduce muscle tightness, improve blood flow, and enhance tissue elasticity.
Silicone’s material properties offer advantages: it is non-porous, reducing bacterial growth; heat-resistant, allowing for sterilization; and durable, ensuring longevity. Additionally, silicone dilators are often designed with ergonomic handles for better grip, and some feature subtle curves to mimic anatomical structures. They are used in various clinical settings, from physical therapy offices to home-based regimens. Unlike dilators of the past, modern silicone versions prioritize patient-centered design, focusing on comfort and usability.
This overview lays the foundation for their applications, emphasizing that they are not mere “tools” but partners in healing, backed by decades of medical research and innovation.
Benefits of Silicone Dilators for Pelvic Floor Health
The benefits of silicone dilators are multifaceted, addressing physical, psychological, and functional aspects of pelvic health.
Firstly, their soft texture minimizes discomfort, encouraging consistent use—a critical factor in rehabilitation. For conditions like vaginismus, where fear of penetration exacerbates muscle spasms, silicone dilators reduce anxiety through gradual exposure.
Secondly, they promote physiological improvements: by stretching tissues, they enhance blood circulation, which aids in healing scar tissue or reducing inflammation post-surgery. Studies, such as those published in the Journal of Sexual Medicine, show that dilator therapy can significantly improve sexual function and reduce pain during intercourse.
Thirdly, silicone dilators offer versatility; they are used for urinary incontinence by relaxing hypertonic muscles, and for pelvic organ prolapse by strengthening support structures.
From a hygiene perspective, silicone is easy to clean with soap and water, lowering infection risks compared to porous materials. Economically, they are cost-effective in the long term, often covered by insurance when prescribed. Psychologically, users report increased confidence and body awareness, as dilators provide tangible progress markers. For clinicians, silicone dilators integrate seamlessly into therapy plans, allowing for personalized progression.
This section elaborates on each benefit with case examples, such as a patient recovering from hysterectomy who regained comfort within weeks, or a vaginismus sufferer achieving pain-free intercourse after months of diligent use. The cumulative evidence underscores why silicone dilators are a cornerstone in modern pelvic health management.
Conditions Treated with Silicone Dilators
Silicone dilators are indicated for a range of pelvic health conditions, each requiring tailored approaches.
Vaginismus is a primary application, where involuntary pelvic muscle contractions prevent penetration. Dilators help desensitize the response through systematic dilation, often combined with cognitive-behavioral therapy. Vulvodynia and vestibulodynia, characterized by chronic vulvar pain, benefit from dilators by improving tissue flexibility and reducing trigger points. Pelvic floor hypertonicity, or excessive tightness, is common in athletes or individuals with stress; dilators relax muscles alongside physical therapy.
Post-surgical recovery is another key area: after procedures like hysterectomy, episiotomy, or gender-affirming surgery, dilators prevent adhesions and maintain vaginal patency. For menopausal women, vaginal atrophy—thinning and dryness due to estrogen loss—can be alleviated with dilators to enhance elasticity. Interstitial cystitis and endometriosis often involve pelvic pain; dilators address comorbid muscle tension. In urinary incontinence, particularly urge incontinence, dilators aid in retraining bladder muscles. Pelvic organ prolapse may use dilators to support pelvic floor exercises. Even pediatric and adolescent cases, such as congenital anomalies, see applications under specialist guidance.
This section details each condition’s pathophysiology, how dilators intervene (e.g., by breaking pain cycles or promoting collagen remodeling), and expected outcomes. Clinical protocols, like starting with the smallest dilator for 10 minutes daily, are discussed, emphasizing the importance of multidisciplinary care involving urologists, gynecologists, and physical therapists.
Several Factors for Choosing the Right Silicone Dilator
Selecting an appropriate silicone dilator is crucial for efficacy and safety. Consider these factors:
Size progression—sets with incremental diameters (e.g., 4-8 pieces) allow gradual adaptation; beginners should opt for sets starting at 0.3-0.5 inches.
Material quality—ensure 100% medical-grade silicone, free from phthalates or latex; certifications like FDA clearance or CE marking add reassurance.
Design features—curved dilators may suit anatomical contours, while straight ones offer simplicity; handles improve control, especially for those with arthritis. Lubrication compatibility—silicone dilators work best with water-based lubricants to avoid material degradation; avoid oil-based products.
Brand reputation—trusted manufacturers like Soul Source, Intimate Rose, or Inspire provide detailed guides and customer support.
Individual needs—for vaginismus, softer, tapered dilators reduce intimidation; for post-surgery, smoother surfaces minimize irritation.
Budget—prices range from $50 to $200; insurance may cover costs with a prescription.
Consultation—always involve a healthcare provider to assess specific conditions and recommend sizes.
This section includes a comparison table of top brands, highlighting pros and cons. For example, Soul Source offers extensive sets with educational materials, while Intimate Rose focuses on ergonomic designs. Additionally, tips on evaluating product reviews and seeking clinical trials data are provided. By making an informed choice, users can avoid common pitfalls like using ill-fitting dilators that cause discomfort or hinder progress.
Step-by-Step Guide to Using Silicone Dilators Safely
Safe usage of silicone dilators hinges on technique, patience, and hygiene. Follow this step-by-step guide:
Preparation: Wash hands and clean the dilator with mild soap and warm water. Pat dry or use a sterilizing solution. Select a private, relaxed space—perhaps with calming music or dim lighting.
Lubrication: Apply a generous amount of water-based lubricant to the dilator tip. Avoid silicone-based lubes unless the dilator is compatible, as they can degrade silicone material.
Positioning: Assume a comfortable position, such as lying on your back with knees bent (lithotomy), sitting with legs apart, or standing with one foot elevated. Use pillows for support.
Relaxation: Practice deep breathing for 5 minutes to ease pelvic tension. Focus on exhaling slowly to release muscle tightness.
Insertion: Gently guide the dilator into the vagina or anus at a slight upward angle toward the tailbone. Proceed slowly; if resistance occurs, pause and breathe until muscles relax. Never force insertion.
Holding: Once inserted, hold the dilator in place for 5-15 minutes, depending on comfort. Gradually increase time over sessions. You may gently rotate or move it to massage tissues.
Progression: After mastering a size, move to the next larger dilator, typically when insertion feels pain-free for consecutive sessions. This may take days or weeks—rushing can cause setbacks.
Aftercare: Remove the dilator slowly, clean it again, and store in a dry container. Note any sensations in a journal to track progress.
Troubleshooting: If pain persists, reduce size or duration; consult a therapist for guidance. Bleeding or severe discomfort warrants medical attention.
This guide emphasizes consistency—daily sessions of 10-20 minutes yield best results. It also covers advanced techniques, such as combining dilation with pelvic floor contractions, to enhance muscle coordination. Safety precautions, like avoiding sharing dilators and checking for material wear, are detailed to prevent infections or injuries.
Integrating Silicone Dilators into Pelvic Floor Therapy
Silicone dilators are most effective when integrated into a holistic pelvic floor therapy program. Pelvic floor physical therapy (PFPT) involves assessment, manual therapy, exercises, and education. Dilators serve as a bridge between clinic and home practice. Initially, a therapist evaluates muscle tone, pain points, and functional goals. For a patient with hypertonic pelvic floor, dilators are introduced to teach relaxation—complementing techniques like biofeedback, where sensors monitor muscle activity. Therapists may guide insertion during sessions, providing real-time feedback on pressure and alignment. In cases of scar tissue from surgery or childbirth, dilators help remodel collagen when used with gentle stretching. A typical protocol includes:
Weeks 1-2: Use the smallest dilator for 10 minutes daily, focusing on breathing.
Weeks 3-6: Progress to larger sizes as tolerated, incorporating Kegel exercises to alternate contraction and relaxation.
Weeks 7-12: Integrate dynamic movements, such as tilting the dilator to address trigger points.
Dilators also enhance other modalities, like electrical stimulation for muscle re-education or ultrasound for pain relief. For sexual dysfunction, therapists may combine dilation with sensate focus exercises. This section includes case studies, like a 35-year-old with vaginismus who, over 6 months of PFPT and dilation, achieved pain-free intercourse. It also discusses collaborative care—therapists working with gynecologists to adjust hormone therapy for atrophic tissues, or with psychologists to address anxiety. Patient education is stressed: understanding the “why” behind dilation improves adherence. By framing dilators as part of a toolkit, rather than a standalone solution, therapy outcomes are optimized, with studies showing success rates exceeding 70% for conditions like vaginismus when combined with multidisciplinary approaches.
Common Myths and Misconceptions About Dilators
Dispelling myths is essential to normalize silicone dilator use.
Myth 1: “Dilators are only for sexual activity.” Reality: They are medical devices for various pelvic disorders, including non-sexual issues like urinary retention.
Myth 2: “Using dilators is painful and traumatic.” Reality: When used correctly with lubrication and gradual progression, discomfort is minimal; pain often stems from improper technique.
Myth 3: “Dilators are a quick fix.” Reality: They require weeks to months of consistent effort, akin to physical therapy for other body parts.
Myth 4: “Dilators are only for women.” Reality: Men use them for pelvic pain, post-prostatectomy recovery, or anal dilation in conditions like fissures.
Myth 5: “Silicone dilators are expensive and inaccessible.” Reality: Many affordable options exist, and insurance coverage is possible with a prescription; community programs may offer subsidies.
Myth 6: “Dilators cause dependency.” Reality: They are temporary aids to achieve long-term muscle health; most users discontinue after goals are met.
Myth 7: “Dilators are embarrassing or shameful.” Reality: Pelvic health is a legitimate medical concern, and tools like dilators should be viewed no differently than crutches for a broken leg.
This section cites expert opinions, such as from the International Pelvic Pain Society, to debunk myths. It also addresses cultural stigmas, encouraging open dialogue through patient testimonials. By confronting misconceptions head-on, we reduce barriers to care and foster a more informed, compassionate approach to pelvic health.
Expert Tips for Maximizing Results
As an expert, JESilicone recommends these evidence-based tips to enhance silicone dilator outcomes:
Consistency Over Intensity: Short daily sessions (10-15 minutes) are more effective than sporadic longer ones. Set reminders or incorporate dilation into a routine, like after showering.
Combine with Pelvic Floor Exercises: Alternate dilation with Kegels—contract muscles for 5 seconds, then relax for 10—to improve strength and flexibility.
Mind-Body Connection: Use mindfulness or meditation apps to reduce anxiety. Visualization techniques, like imagining muscles “melting,” can ease insertion.
Thermal Therapy: Apply a warm pad to the pelvic area before dilation to increase blood flow and relax muscles.
Journaling: Track progress, noting sizes used, pain levels (on a scale of 1-10), and emotional states. This identifies patterns and motivates persistence.
Professional Guidance: Schedule regular check-ins with a therapist to adjust plans. Telehealth options offer convenient support.
Lubrication Choices: Experiment with different water-based lubricants; some contain aloe vera or hyaluronic acid for added moisture.
Position Variability: Try different positions—side-lying may reduce pressure for some, while squatting can open the pelvic floor.
Community Support: Join online forums or support groups (e.g., through the National Vulvodynia Association) for shared experiences and encouragement.
Patience and Self-Compassion: Progress may be nonlinear; celebrate small victories, like tolerating a larger size for an extra minute.
These tips are grounded in clinical practice, with research showing that multimodal approaches yield higher success rates. For instance, a 2020 study in the American Journal of Obstetrics and Gynecology found that combining dilation with mindfulness reduced pain scores by 40% in pelvic pain patients. This section elaborates on each tip with practical examples, such as how to integrate dilation into a busy schedule or troubleshoot plateaus.
Frequently Asked Questions (FAQs) About Silicone Dilators
Q1: How long until I see results with silicone dilators?
A: It varies by condition—vaginismus may show improvements in 4-8 weeks, while post-surgical recovery can take 3-6 months. Consistency is key.
Q2: Are silicone dilators safe during pregnancy or postpartum?
A: Consult your doctor; generally, they are safe postpartum for scar management, but avoid during pregnancy unless prescribed for specific conditions.
Q3: Can I use silicone dilators with condoms or other devices?
A: Yes, but ensure condoms are non-lubricated or water-based to prevent silicone degradation. Avoid combining with electrical devices without professional advice.
Q4: How do I clean and store silicone dilators?
A: Wash with mild soap and water after each use, or use a sterilizing solution like hydrogen peroxide. Store in a clean, dry case away from direct sunlight.
Q5: What if I experience pain or bleeding?
A: Stop immediately; pain may indicate incorrect size or technique. Bleeding could signal tissue damage—consult a healthcare provider to rule out underlying issues.
Q6: Are there alternatives to silicone dilators?
A: Yes, plastic or glass dilators exist, but silicone is preferred for flexibility. Balloon dilators or finger stretching are other options under guidance.
Q7: Can men use silicone dilators?
A: Absolutely—for anal dilation in pelvic pain or post-surgery, or urethral dilation for strictures, always with medical supervision.
Q8: How often should I replace my dilator?
A: With proper care, silicone dilators last years. Replace if you notice cracks, discoloration, or loss of elasticity.
Q9: Do I need a prescription to buy silicone dilators?
A: In many countries, no, but a prescription helps with insurance reimbursement and ensures professional fitting.
Q10: Can dilators be used for sexual pleasure?
A: While primarily medical, they may aid in sexual health by reducing pain, but consult a therapist for personalized advice.
This FAQ section is based on common queries from my practice, offering concise answers to empower users with confidence.
Conclusion: Empowering Your Pelvic Health Journey
Silicone dilators represent a paradigm shift in pelvic health, offering a compassionate, evidence-based approach to healing. From alleviating pain to restoring function, their benefits are profound and far-reaching. As an manufacturing expert, JESilicone urges individuals to view these tools not as a last resort, but as proactive steps toward wellness. Embrace the journey with patience—pelvic health is a marathon, not a sprint. Collaborate with healthcare providers, leverage community resources, and trust in your body’s resilience. Remember, conditions like vaginismus or pelvic pain are treatable, and silicone dilators are a testament to medical innovation prioritizing patient comfort.
By integrating the insights from this guide—from choosing the right dilator to debunking myths—you are equipped to navigate your path with knowledge and agency. Let this be a call to action: prioritize your pelvic health, break the silence, and explore the transformative potential of silicone dilators. Together, we can foster a world where pelvic wellness is accessible, understood, and celebrated.